“Was the government to prescribe to us our medicine and diet, our bodies would be in such keeping as our souls are now.” —Thomas Jefferson, 1782
I saw a clip of Dr. Leonard Coldwell on Facebook talking about the medical profession and shared it. A Facebook friend asked me if I believed what Coldwell was saying. I told my friend that I would blog about it. The short answer is that there is something to what Coldwell is saying. But a longer answer is required to fully address the matter.
Here’s the clip: https://www.facebook.com/reel/1257189255629566
I am not here to judge Coldwell. I know very little about him other than the mainstream medical science establishment has determined that he is problematical and social media platforms have been censoring him. My aim in this essay is to look into what he said in the video clip—that the modern medical profession is not interested in curing or preventing illness but only in treating it—and see if there is anything to his claims. He argues that there is no money to be made from curing or preventing illness; on the other hand, there is plenty of money to be made from addressing symptoms. He moreover makes the claim that physicians are at a high risk of suicide, and that’s because they come to realize that they have been pulled into a profession that is interested not in the wellbeing of those seeking help but in generating trillions of dollars by perpetuating disease.

Coldwell’s account concerns Andrew Carnegie, a Scottish immigrant who became one of the wealthiest individuals in the United States during the Gilded Age (John D. Rockefeller plays a role in this, as well, which I will come to later). Carnegie played a significant role in the development of medical education in America and thus contributed in a signifiant way to the trajectory of the medical industry. The story one usually hears about this is a celebration of philanthropic endeavors, but as usual there’s more to the story. Whatever else Coldwell says about medicine, he is onto something here.
The story begins in 1908, when the American Medical Association (AMA) and Council on Medical Education (CME) asked the Carnegie Foundation to investigate the allegedly appalling state of medical education. The standard narrative goes like this: back then, medical schools across the nation operated with minimal standards, lacked rigorous curricula, and were poorly regulated; graduates from these schools were inadequately prepared to practice medicine. So, Carnegie, along with other philanthropic industrialists of the time, funded initiatives to reform the education. This was one of the many blooms of progressivism.
One of Carnegie’s key contributions was the Carnegie Foundation for the Advancement of Teaching, established in 1905. This drew the AMA and CME to Carnegie. Under the leadership of Abraham Flexner, the Carnegie Foundation funded the Flexner Report (1910), which evaluated medical schools across the US and Canada. The report purported to have exposed deficiencies in medical education and called for numerous reforms, including the establishment of higher standards for admission, curriculum requirements, and clinical training (see The Flexner Report ― 100 Years Later).
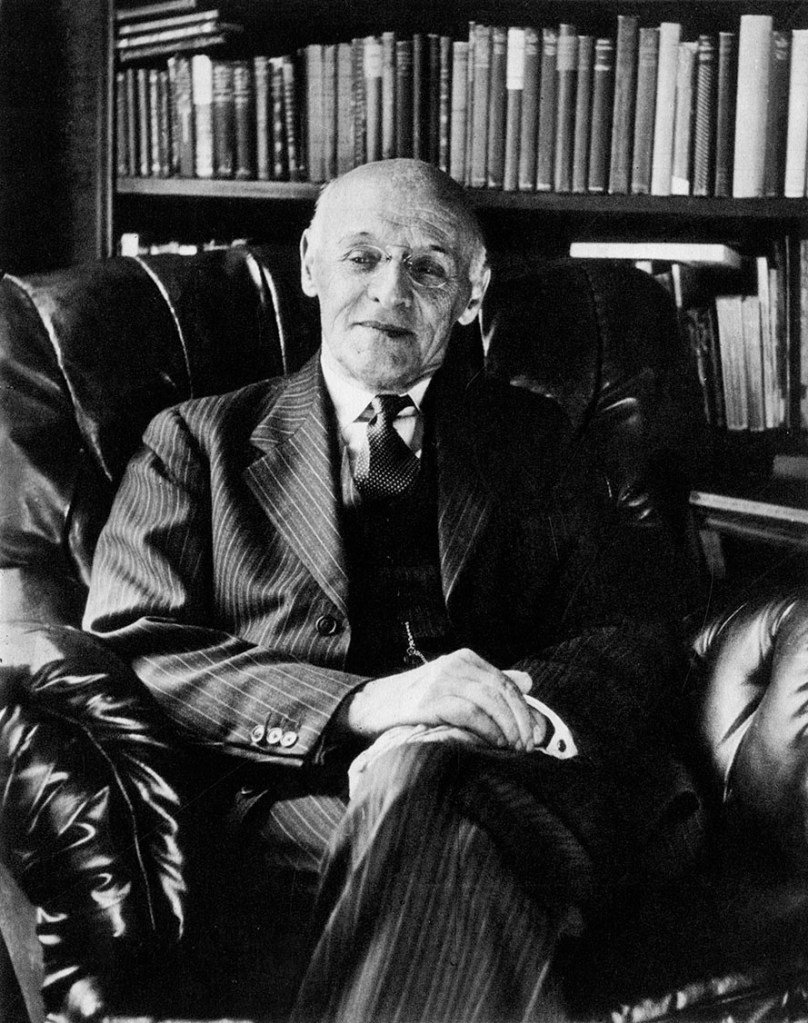
The Flexner Report had a transformative effect on medical education in the United States. It led to the closure of medical schools and encouraged the development of more rigorous programs that aligned with “scientific” approaches to medicine. While improving certain aspects of medical education, the main effect of the Flexner Report was to reinforce a system that emphasized the management of disease rather than its cure and prevention. Medical professionals were trained to rely heavily on pharmaceutical treatments, surgical interventions, and technological solutions, rather than addressing the root causes of diseases, particularly in a holistic manner.
The Flexner reforms thus professionalized medicine in a way that centered the role of the physician as a highly trained specialist focused more on the technical aspects of treatment rather than the overall wellbeing of the patient. This approach turned medical care into a business that emphasized disease management, often with costly interventions. The medical model that emerged from these reforms conditioned physicians to ignore factors like lifestyle; doctors were trained to treat diseases as isolated conditions rather than considering the behavioral, environmental, and social factors associated with health, illness, and wellbeing. Furthermore, the reforms led to a consolidation of medical schools and the closure of smaller, often alternative institutions, which reduced diversity of medical education, limiting the incorporation of holistic healing practices that may have been more focused on treating diseases in a non-invasive way.
The system that emerged from the Flexner reforms ultimately became one that was aligned with corporate interests, as pharmaceutical companies and the growing healthcare industry became central to the medical field. Put another way, the Flexner reforms were an important factor in the emergence of what I have called the “medical-industrial complex.” (For some of my essays concerning the medical industry see Making Patients for the Medical-Industrial Complex; Feeding the Medical-Industrial Complex; Thomas Szasz, Medical Freedom, and the Tyranny of Gender Ideology; The Science™ and its Devotees; Fear and Loathing in the Village of Chamounix: Monstrosity and the Deceits of Trans Joy; The Persistence of Medical Atrocities: Lobotomy, Nazi Doctors, and Gender Affirming Care; Disordering Bodies for Disordered Minds.)
Let’s go a deeper. Throughout history, the medical field has been marked by a tension between two competing approaches to healthcare. On one side are the allopaths who in the eighteenth and nineteenth centuries employed aggressive methods such as bloodletting, the use of toxic agents like arsenic and mercury, and radical surgeries to treat disease. These techniques, grounded more in “scientific” theory than empirical evidence, aimed to forcibly expel illness from the body. To be sure, the specific methods of the allopaths have changed over the decades (arsenic and mercury have been replaced by antibiotics and antiviral agents), but the aggressive approach to medicine at the expense of healing and prevention remains the central characteristic of allopathy. On the other side are the naturopaths, who advocate time-tested treatments based on empirical observation. Their methods, including the use of plants, nutrition, and practices that support the body’s natural defenses, emphasize healing from within.
These two approaches rest on different but complementary theories of disease. The germ theory of disease, foundational to modern allopathic medicine, posits that microorganisms such as bacteria and viruses are the primary causes of illness. Following from this, allopathy focuses on diagnosing and treating diseases by targeting their specific pathogenic agents through interventions like antibiotics, antivirals, vaccines, and surgical procedures. Allopaths tend to isolate disease causation to external agents, often neglecting the broader environmental and social conditions that create fertile ground for the spread of pathogens. For instance, while medications address immediate threats, germ theory’s narrow focus overlooks systemic factors like overcrowding, poor sanitation, or unequal access to healthcare that perpetuate disease vulnerability. For example, much of the reduction in death and serious illness associated with various pathogens, such as measles, is less attributable to vaccines than to improving living conditions brought about by growing affluence and the successes of the workers movement.
In contrast, the terrain theory of disease, aligned with naturopathy, emphasizes the internal and external environments that influence an individual’s health. Terrain theory argues that pathogens are not the sole or even the primary cause of illness but become harmful when the body’s internal “terrain” is weakened due to imbalances in immune function, nutrition, and stress. Naturopathy recognizes that the external environment and social factors are major factors in disease production; health is profoundly shaped by chronic stress, living conditions, access to clean water and air, socioeconomic realities such as poverty. These intersect to create conditions in which pathogens can thrive. In practice, naturopathy prioritizes prevention and wellness by addressing these underlying factors, promoting dietary changes, and stress management (and the elimination of stressors), as well as advocating for systemic reforms to improve the broader environmental and social conditions that undermine public health.
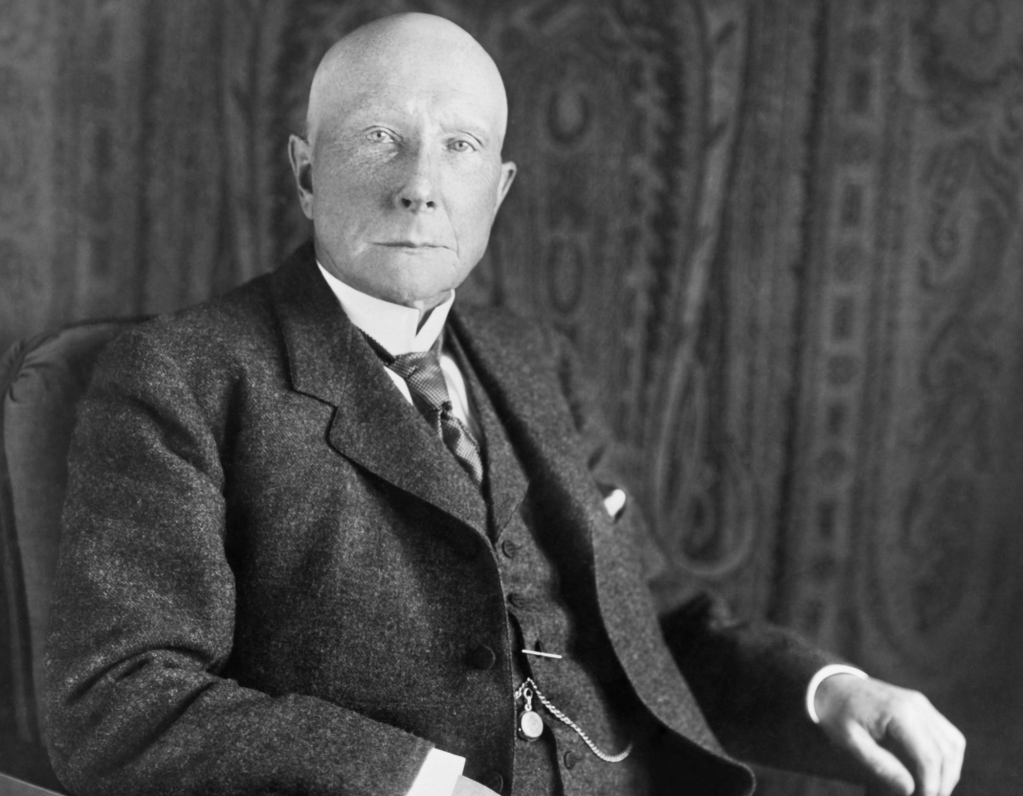
The competition between these theories and approaches persisted until the Flexner Report. Together, these perspectives suggested that, while germ theory and allopathy are effective in acute interventions, terrain theory and naturopathy provides a holistic framework for fostering resilience and addressing the root causes of disease. However, while both schools of thought had profitable practices, the rise of petrochemicals and the advent of synthetic materials hinted at lucrative possibilities in pharmaceutical production and other artificial therapies, and the drive to maximize profits found allopathy and the germ theory of disease to be the best fit for the medical industrial model. John D. Rockefeller recognized the financial potential in allopathic medicine and encourage Andrew Carnegie to join him in creating an environment in which that potential could be realized. It was Carnegie who commissioned Abraham Flexner to assess medical schools across North America and the prevailing medical practices of the day. (The Flexner Report of 1910 and Its Impact on Complementary and Alternative Medicine and Psychiatry in North America in the 20th Century.)
One focus of the Flexner Report was on discrediting naturopathic medicine, branding it as “quackery,” which capitalism’s money power and the emerging regulatory apparatus seized upon to push naturopathy and the terrain theory of disease to the margins. Medical schools offering natural treatments faced closure unless they conformed to the allopathic model, losing accreditation and funding if they resisted. As a result, countless doctors lost their livelihoods, and hospitals and schools rooted in naturopathy were shuttered. Rockefeller, under the guise of philanthropy, donated tens of millions of dollars to colleges and hospitals, ensuring compliance with the report’s recommendations and building up the infrastructure to change medicine from the ground up. He established the General Education Board to oversee medical education, effectively centralizing control over the profession.
Meanwhile, pharmaceutical companies entrenched their influence by incentivizing doctors to prescribe their products, creating a system where quick prescriptions replaced holistic patient care. Organizations like the American Medical Association (AMA) further entrenched allopathy’s dominance, lobbying government to marginalize natural practices. Regulatory hurdles imposed by the Food and Drug Administration (FDA) made it nearly impossible for natural remedies to gain approval, as herbs and supplements could not be patented and thus lacked the financial backing necessary to meet the FDA’s costly standards.
This corporatized system is the structure of modern medicine, which, while effective in many areas, prioritizes symptom management over addressing root causes, ensuring a steady profit stream from managing chronic disease. Rising healthcare costs and insurance mandates exacerbate the issue, creating a cycle of dependency that benefits pharmaceutical companies and entrenched medical institutions.
As I have argued in past writings, just as the military-industrial complex needs war to sell weapons and military hardware, so the medical-industrial complex needs sickness to sell pharmaceuticals, surgeries, and therapies. And the foods industry assists in maintaining an unhealthy population. The problem is systemic, a vast structure driven by profit over patient wellbeing.
Consider, for example, diabetes rates in the United States, which have increased significantly over the past few decades. Over the last two decades, the number of American adults with diabetes has more than doubled, rising from around eleven million to over 23 million (according to the CDC). When including undiagnosed cases, the total prevalence exceeds 37 million people, representing more than eleven percent of the entire US population. If we don’t change course, by 2025, projections suggest that more than 50 million Americans could have diabetes, with around 15 percent of the population expected to have a diagnosed case.
What has produced this health crisis? Poor diet and a sedentary lifestyle among other things. There’s no money in addressing these problems. But there is money to be made from Ozempic, a diabetes treatment developed by Novo Nordisk, which is projected to enjoy significant revenue growth due to the expanding use of its product for type two diabetes and off-label applications like weight loss. Sales of the drugs are in the billions.
The medical-industrial complex, far from improving the health of the populace is a cause of disease and death. A 2016 analysis by researchers at Johns Hopkins University estimated that medical errors cause 250,000 deaths annually, making it the third leading cause of death in the United States after heart disease and cancer. This estimate is based on hospital data and includes errors such as misdiagnoses, medication mistakes, surgical errors, and communication breakdowns within the healthcare system.
A 1998 meta-analysis in the Journal of the American Medical Association (JAMA) estimated that serious adverse drug reactions caused approximately 106,000 deaths annually in hospitalized patients. More recent estimates likely exceed this figure due to the increased use and overprescribing of medications, particularly in an aging population. The Lown Institute has documented the harms of overtreatment, with estimates suggesting thousands of deaths occur annually due to inappropriate therapies, such as unnecessary stent placements, back surgeries, or aggressive end-of-life interventions.
Carnegie did not explicitly label himself as a progressive in the political sense, but his beliefs and actions aligned with progressive ideals—and this includes his support for eugenics. Carnegie funded the Carnegie Institution for Science, which included the Eugenics Record Office, a center for eugenics research led by Charles Davenport. Likewise, the Rockefeller Foundation funded studies at the Kaiser Wilhelm Institute in Germany, which later became associated with Nazi racial policies. Eugenics and progressivism share an interest in improving society through rational planning and scientific management. To draw attention away from the real causes of inequality, mainly the exploitation of labor under capitalism, many progressives embraced eugenics as a way to address social issues like crime, disease, and poverty, believing that selective breeding could eliminate the undesirable traits they asserted as the real cause of these problems.
I raise the matter of eugenics to help the reader understand the motives of industrialists like Carnegie and Rockefeller, but also to return to one of the central themes on Freedom and Reason, and that is the dark reality of progressivism, with its emphasis on expertise and social engineering and the necessity of coercive policies (see, for example, On the Ethics of Compulsory Vaccination; “Three generations of imbeciles are enough”; Biden’s Biofascist Regime). In the pursuit of the corporate state, individuals lives are rather insignificant (forever wars testify to this). The medical industry kills, maims, and sickens millions of people every year, but this is of little concern if there is a profit to be made. The focus on the individual as the center of disease and other maladies rather than the social conditions that underpin what are really social problems functions to obscure the role that the capitalist mode of production plays in human misery. Fixing the problems of the capitalist mode of production beyond ameliorating some of its worst excesses is more than unprofitable; it means jettison the system altogether.
Finally, Coldwell’s claim that doctors have a higher suicide rate compared to the general population is accurate. This phenomenon has been well-documented in various studies and is a significant concern within the medical community. According to research, the suicide rate among male physicians is 1.5 times higher than the general male population, while female physicians have a rate that is 2-4 times higher than the general female population. Estimates suggest that 300-400 physicians die by suicide annually in the United States. This is true for nurses, as well. In a 2020 study published in JAMA Psychiatry, researchers found that the suicide rate among nurses was 23.8 per 100,000 compared to 16.1 per 100,000 in the general population.

True reform requires public awareness and a willingness to challenge the status quo. By embracing natural remedies, prioritizing preventative care, and educating themselves about their health, individuals can begin to reclaim autonomy over their well-being. This is what Robert Kennedy, Jr’s “Make America Healthy Again” (or MAHA) campaign endeavors to accomplish. It does not mean turning our backs on the strengths of allopathic medicine. It means bringing theory and practice under the control of a democratically-controlled public health system focused on diet, the environment, and social conditions, and this means moving away from the for-profit medical model towards a community-based model based on a holistic approach to health and wellbeing.